The stylomastoid foramen is a small but important part of our body. It’s found between the styloid and mastoid processes of the temporal bone. It lets the facial nerve and stylomastoid artery pass through. This is key for controlling our facial expressions and other functions.
Knowing about the stylomastoid foramen’s anatomy is key for diagnosing and treating problems. The plicae semilunares, or synovial folds, in places like the knee joint are similar to the structures around the stylomastoid foramen.
The link between the stylomastoid foramen and other body parts shows how complex and connected our anatomy is.
Overview of Craniofacial Anatomy
The craniofacial region is a complex area. It includes the skull and face bones, neural pathways, and blood vessels. These structures are key for our senses and movement.
Temporal Bone Structure and Function
The temporal bone is vital in the craniofacial area. It houses parts of the ear and balance systems. It has different parts like the squamous and petrous portions.
Each part has its own role. The temporal bone protects the ear’s delicate structures. It helps with hearing and balance.
Key Neural Pathways in the Facial Region
The face is full of nerves that control our expressions and senses. Knowing these nerves is key for face health issues.
Cranial Nerve Distribution
The facial nerve (CN VII) controls face muscles. Its branches and connections are complex. They allow for facial movements and taste.
The craniofacial area’s anatomy is complex. Knowing the temporal bone and nerves is important for doctors and researchers.
Stylomastoid Foramen: Definition and Location
The stylomastoid foramen is a key spot between the styloid and mastoid processes of the temporal bone. It’s a passageway for important nerves, like the facial nerve.
Anatomical Position in the Temporal Bone
The stylomastoid foramen is found in the temporal bone. This bone is complex and houses ear structures. It’s vital for understanding cranial anatomy.
Surrounding Structures and Relationships
The stylomastoid foramen is near many important landmarks. Its spot between the styloid and mastoid processes is key to understanding its role.
Proximity to Mastoid Process
The mastoid process is a bony part behind the ear. It’s close to the stylomastoid foramen. This closeness is important for surgeries and tests.
Relationship to Styloid Process
The styloid process is a long, thin bone. It’s also near the stylomastoid foramen. This shows its place in the temporal bone’s complex anatomy.
| Anatomical Landmark | Relation to Stylomastoid Foramen |
|---|---|
| Mastoid Process | Located posteriorly to the stylomastoid foramen |
| Styloid Process | Located anteriorly to the stylomastoid foramen |
| Facial Nerve | Passes through the stylomastoid foramen |
Knowing where the stylomastoid foramen is and its connections is key. It’s important for both learning anatomy and for medical work. Its role in carrying the facial nerve makes it very important in neuroanatomy.
Embryological Development of the Stylomastoid Foramen
The stylomastoid foramen develops during a certain time in fetal growth. It’s shaped by many factors in embryology. This is key for the facial nerve and nearby areas to form right.
Formation During Fetal Development
In fetal growth, the stylomastoid foramen comes into being. It’s a result of the temporal bone and facial nerve working together. The facial nerve, or cranial nerve VII, goes through this foramen. The foramen’s creation is tied to the temporal bone’s growth, like the mastoid and styloid processes.
Developmental Variations and Anomalies
There can be differences in how the stylomastoid foramen develops. These differences might show in its size or where it is. Such variations can affect the facial nerve and its work.
Clinical Implications of Developmental Variations
It’s important for doctors to know about these developmental differences. Understanding these can help in diagnosing and treating facial nerve issues. For example, a foramen that’s too big or small can make the nerve more prone to damage.
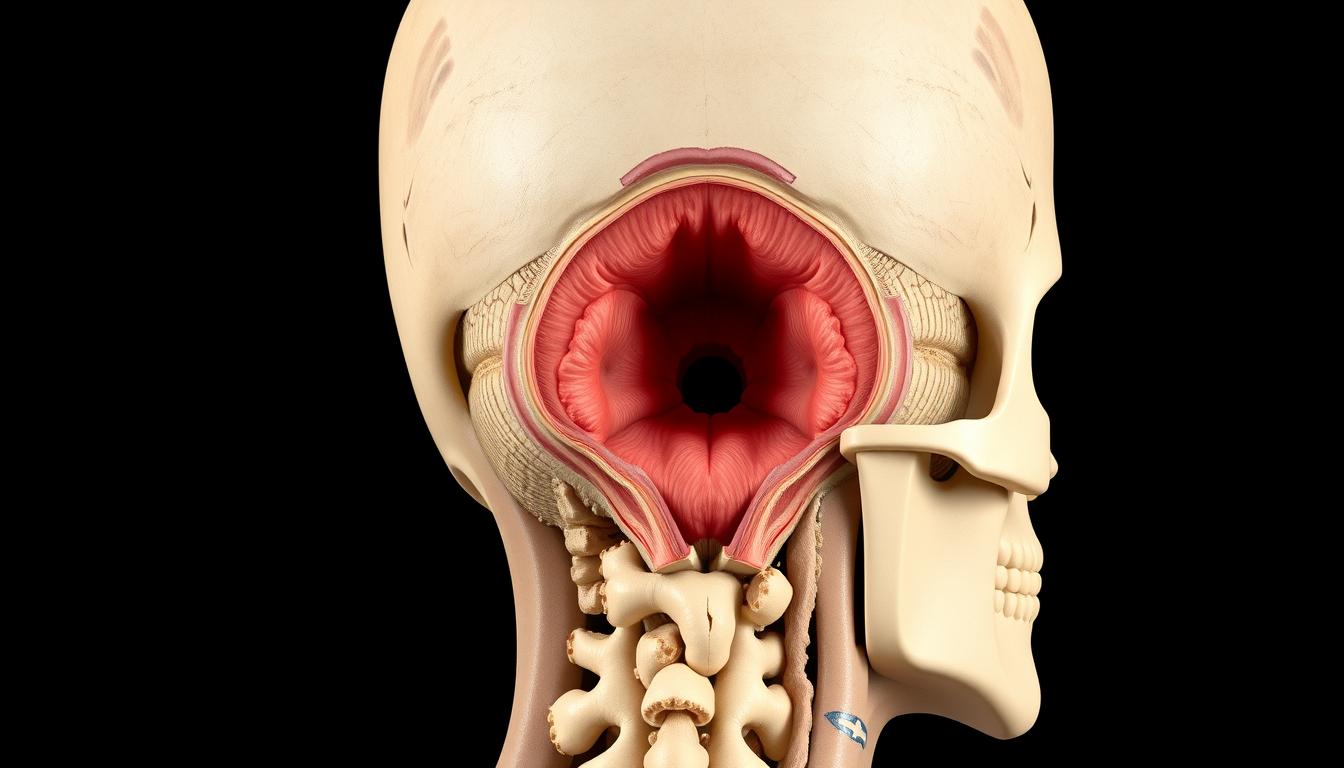
Structures Passing Through the Stylomastoid Foramen
The stylomastoid foramen is key for nerves and vessels to pass through. It’s vital for the facial nerve and blood vessels to work right.
Facial Nerve (CN VII) Anatomy
The facial nerve, or cranial nerve VII, controls facial expressions and taste. It exits the skull through the stylomastoid foramen. Here, it branches out to muscles of facial expression.
The facial nerve’s anatomy is complex. It has a winding path through the temporal bone before it comes out at the stylomastoid foramen. Knowing this is key for treating facial nerve problems.
Stylomastoid Artery
The stylomastoid artery comes from the posterior auricular artery. It supplies blood to the facial nerve and nearby areas as it goes through the foramen. This artery is important for the facial nerve’s health.
Associated Venous Structures
Venous structures go with the facial nerve and stylomastoid artery through the foramen. They help with drainage. These veins are part of a network that ensures blood flows back from the face.
Neurovascular Bundle Organization
The neurovascular bundle in the stylomastoid foramen is very organized. The facial nerve, stylomastoid artery, and veins are arranged in a special way. This helps them pass through and function well.
The exact way these structures are arranged is very important. Any problem can cause big issues.
Clinical Significance of the Stylomastoid Foramen
The stylomastoid foramen is key in otologic surgery and facial nerve issues. Its spot at the mastoid and styloid processes junction is vital for surgeons and doctors.
Role in Facial Nerve Disorders
The stylomastoid foramen is closely tied to the facial nerve (CN VII). This nerve leaves the skull through this foramen. Issues like Bell’s palsy or injuries often happen here.
Knowing the anatomy of this area is key for diagnosing and treating facial nerve problems.
Some important points about facial nerve issues near the stylomastoid foramen include:
- Compression or injury to the facial nerve as it exits the foramen
- Infection or inflammation affecting the nerve within the foramen
- Tumors or growths near the stylomastoid foramen that may compress the facial nerve
Surgical Considerations and Approaches
Surgeries near the stylomastoid foramen need exact anatomy knowledge to avoid problems. The foramen is a key point for mastoidectomies and facial nerve decompression.
Landmark Importance in Otologic Surgery
In otologic surgery, the stylomastoid foramen helps find the facial nerve. Surgeons must know its location and its relation to other structures. This helps them navigate the complex temporal bone anatomy.
“The stylomastoid foramen is a critical anatomical landmark that guides surgeons during otologic procedures, helping to preserve the integrity of the facial nerve.”
Understanding the stylomastoid foramen’s clinical importance helps healthcare professionals. They can improve their skills in diagnosing and treating facial nerve disorders or otologic surgery. This leads to better patient outcomes.
Pathologies Related to the Stylomastoid Foramen
Understanding the pathologies related to the stylomastoid foramen is key for diagnosing and treating facial nerve disorders. The stylomastoid foramen is a critical passage for the facial nerve. It can be affected by various conditions that impact its function and the overall health of the individual.
Bell’s Palsy and Facial Nerve Compression
Bell’s palsy is a common condition that causes sudden weakness or paralysis of the facial muscles. It usually affects one side of the face. Symptoms include drooping eyelids, difficulty closing the eye, and drooling. The exact cause is often unknown, but viral infections are thought to play a role.
To diagnose Bell’s palsy, doctors rule out other causes of facial weakness. Treatment includes corticosteroids to reduce inflammation and, in some cases, antiviral medications.
Trauma and Fractures Affecting the Region
Trauma to the temporal bone can result in fractures that affect the stylomastoid foramen and the facial nerve. Fractures can cause compression or transection of the nerve, leading to facial paralysis or weakness. The severity of the injury determines the treatment approach, which may include surgical intervention to relieve pressure on the nerve or repair damaged nerve fibers.
- Temporal bone fractures can be classified into longitudinal, transverse, or mixed types, each with different implications for the facial nerve.
- Prompt diagnosis and management are critical to prevent long-term damage.
Tumors and Growths Near the Foramen
Tumors or growths near the stylomastoid foramen can compress or invade the facial nerve. Benign tumors, such as schwannomas or parotid gland tumors, are among the possible growths that can affect this region.
Diagnostic Approaches for Stylomastoid Region Disorders
Diagnosing disorders related to the stylomastoid foramen involves a combination of clinical evaluation, imaging studies, and sometimes electrophysiological tests. MRI and CT scans are commonly used to visualize the anatomy and identify any abnormalities. Electromyography (EMG) and nerve conduction studies can assess the function of the facial nerve.
| Diagnostic Tool | Purpose |
|---|---|
| MRI | Visualize soft tissue abnormalities, including tumors or inflammation. |
| CT Scan | Assess bony structures and detect fractures or other bony abnormalities. |
| EMG/Nerve Conduction Studies | Evaluate the function of the facial nerve and muscle activity. |
Transitioning from Cranial to Appendicular Anatomy
When we move from studying the head to the limbs, it’s key to see how they connect. The head’s anatomy, like the stylomastoid foramen, is vital for our body’s functions. Yet, the limbs and their parts are just as important.
It’s important to note the role of special structures when moving between these areas. For example, the knee’s synovial joints are found throughout our body.
Comparative Importance of Specialized Anatomical Structures
Special structures, like the stylomastoid foramen and knee synovial joints, show the complexity of human anatomy. Each has its own function, essential for our health.
Synovial Structures Throughout the Body
Synovial structures, including joints and folds, are found all over. In the knee, plicae semilunares are key for joint movement and fluid distribution.
Here are some key points about synovial structures:
- Synovial joints allow for a wide range of motion.
- Synovial folds, like plicae semilunares, help with joint health by distributing fluid.
- Different joints and body parts have varying amounts of synovial structures.
Plicae Semilunares: Definition and Classification
Plicae semilunares, or synovial folds, are key to the knee’s function and health. They are leftover from when we were embryos. Knowing about them is vital for understanding the knee and treating it.
Types of Synovial Folds in the Knee
The knee has different kinds of synovial folds. They are named based on where they are and what they look like. The main types are:
- Medial plica
- Suprapatellar plica
- Infrapatellar plica
- Lateral plica
Each type has its own features and can cause different problems.
Anatomical Variations of Plicae
Plicae semilunares vary a lot from person to person. These differences can change how big or shaped they are. It’s key to know these differences for correct diagnosis and treatment.
Prevalence in Different Populations
Studies show that plicae semilunares are more common in some groups than others. For example, some groups might have more of certain types. This is something doctors should think about when they’re looking at patients.
A study found that how common plicae semilunares are can vary a lot. This means each person needs a treatment plan that’s just for them.
“The anatomical variations of plicae semilunares underscore the complexity of knee joint anatomy and the need for nuanced clinical approaches.”
Anatomy of Plicae Semilunares in the Knee Joint
Knowing about plicae semilunares is key to treating knee problems. These are folds in the knee’s synovial membrane. They can lead to various knee issues. Each type of plica has its own structure and location in the knee.
Medial Plica Structure and Position
The medial plica is often talked about because it can cause pain. It’s found on the knee’s inner side. Its structure varies, which affects its role in knee health.
Suprapatellar Plica Anatomy
The suprapatellar plica is a significant fold above the patella. It can look like a problem on scans. Knowing its anatomy helps doctors diagnose and treat correctly.
Infrapatellar Plica Characteristics
The infrapatellar plica, or ligamentum mucosum, is below the patella. It’s not as common a cause of symptoms as the medial plica. Yet, it’s important for knee function.
Lateral Plica Considerations
Lateral plicae are not as often discussed but are vital in knee anatomy. They’re on the knee’s outer side and can be part of knee problems.
Histological Features of Synovial Plicae
Synovial plicae have a thin synovial layer over a fibrous core. Their histology helps us understand their role and how they might get involved in diseases. Key features include:
- A thin synovial lining
- A fibrous core that provides structural support
- Vascular elements that contribute to their metabolic activity
In summary, plicae semilunares are complex and varied. Each type has unique features and implications for knee health. Understanding them is vital for diagnosing and treating knee issues.
Physiological Function of Plicae Semilunares
Understanding plicae semilunares is key to knowing how the knee works. These are folds of tissue in the knee. They help the knee move smoothly and stay healthy.
Role in Knee Joint Mechanics
Plicae semilunares help the knee move well by moving the synovial membrane. They reduce friction, making the knee work better. Their condition affects how the knee bends and straightens.
Contribution to Synovial Fluid Distribution
They also help spread synovial fluid in the knee. This fluid keeps the joint lubricated and nourishes the cartilage. Even distribution of this fluid keeps the joint healthy and prevents arthritis.
Proprioceptive Functions
Plicae semilunares have another role too. They have nerve endings that send signals about the joint’s position and movement. This helps with movement coordination and keeps the joint stable.
Evolutionary Perspectives on Plicae
From an evolutionary view, plicae semilunares help the knee work better and last longer. They are found in many species, showing their importance for joint function and mobility.
| Function | Description |
|---|---|
| Mechanical | Facilitates smooth movement and reduces friction |
| Synovial Fluid Distribution | Ensures even distribution of synovial fluid |
| Proprioceptive | Provides sensory feedback for joint position and movement |
Plica Syndrome: Pathophysiology and Presentation
Irritation and inflammation of the plicae semilunares cause plica syndrome. This condition affects knee function and is a major source of knee pain. It mainly affects people who do activities that bend and straighten the knee a lot.
Mechanisms of Plica Irritation and Inflammation
The plicae semilunares can get irritated by overuse, trauma, or repetitive strain on the knee. When they get inflamed, they can cause pain and discomfort, mainly when bending the knee.
The reasons behind plica irritation are complex. They involve how the synovial tissue interacts with the knee’s structures. Synovial inflammation can make the plicae thicker, leading to mechanical irritation and pain.
Clinical Symptoms and Physical Examination
People with plica syndrome often have medial knee pain. This pain gets worse with activities like squatting or climbing stairs. A physical exam might show tenderness on the medial patellar edge. Sometimes, a palpable snapping or clicking sensation is felt.
Doctors check knee mobility, pain location, and mechanical symptoms. A detailed exam helps tell plica syndrome apart from other knee pain causes.
Differential Diagnosis from Other Knee Conditions
Other knee conditions like patellofemoral pain syndrome, meniscal tears, and ligament sprains can be confused with plica syndrome. A thorough clinical evaluation and sometimes imaging studies are needed for accurate diagnosis.
| Condition | Common Symptoms | Diagnostic Clues |
|---|---|---|
| Plica Syndrome | Medial knee pain, snapping sensation | Tenderness over medial patellar edge |
| Patellofemoral Pain Syndrome | Anterior knee pain, crepitus | Pain on patellar compression |
| Meniscal Tears | Pain on knee rotation, locking sensation | Positive McMurray’s test |
Risk Factors for Plica Syndrome Development
Several factors increase the risk of getting plica syndrome. These include repetitive knee activities, direct trauma to the knee, and abnormal knee mechanics. Knowing these risk factors helps in prevention and management.
- Repetitive knee flexion and extension
- Direct trauma to the knee
- Abnormal knee mechanics or alignment
Diagnostic Approaches for Plicae-Related Disorders
Understanding knee anatomy is key to diagnosing plicae-related disorders. Plicae are folds in the knee that can cause symptoms if irritated or inflamed.
Imaging Techniques for Plica Identification
Magnetic Resonance Imaging (MRI) is vital for spotting plicae-related issues. It shows the folds’ thickness and any inflammation. MRI also helps rule out other knee problems with similar symptoms.
Arthroscopic Evaluation and Findings
Arthroscopy is the top method for diagnosing plica syndrome. It lets doctors see the plicae up close. They can check for inflammation and tenderness during the procedure.
“Arthroscopy provides a definitive diagnosis by directly visualizing the plica and assessing its pathology.”
Clinical Tests and Assessment Methods
Clinical tests are key for diagnosing plicae issues. Patients often feel pain in the medial knee, worse when bending. The medial plica shelf test is used to check for plica syndrome. Other signs include tenderness and a cord-like feeling along the joint line.
Emerging Diagnostic Technologies
New technologies like ultrasound and advanced MRI are being looked into. They might offer non-invasive ways to diagnose plicae problems.
Treatment and Management of Plica Syndrome
Dealing with plica syndrome needs a full plan, with both non-surgical and surgical steps. The right choice depends on how bad the symptoms are and how they affect daily life.
Conservative Management Approaches
First, doctors often try non-surgical ways to treat plica syndrome. This includes physical therapy to strengthen the knee muscles and improve flexibility. Anti-inflammatory medications might also be used to control pain and swelling.
It’s important to rest and avoid activities that make the problem worse. This means staying away from bending the knee a lot or putting direct pressure on it.
Surgical Interventions and Techniques
If non-surgical methods don’t work, surgical intervention might be needed. Arthroscopic surgery is often used. It lets doctors look at and treat the plica with a small incision. The goal is to remove or release the irritated plica to ease symptoms.
Rehabilitation Protocols and Outcomes
After surgery, a good rehab plan is key for the best results. This includes exercises to get the knee working right again. The aim is to get the patient back to their usual activities without pain.
Prevention Strategies for Athletes and Active Individuals
For athletes and those who do a lot of activities that stress the knee, prevention is important. This means using the right training methods, doing strengthening exercises, and wearing the right protective gear.
Recent Advances in Treatment Modalities
New ways to treat plica syndrome include better arthroscopic techniques and biologic treatments. These help with healing and reducing swelling. They offer new hope for those with this condition.
| Treatment Approach | Description | Outcome |
|---|---|---|
| Conservative Management | Physical therapy, anti-inflammatory medications, rest | Symptom reduction, improved knee function |
| Surgical Intervention | Arthroscopic surgery to remove or release irritated plica | Alleviation of symptoms, restoration of knee function |
| Rehabilitation Protocols | Structured exercises to restore strength and range of motion | Return to normal activities without pain |
Conclusion
The human body’s details, like the stylomastoid foramen and plicae semilunares, are key to understanding health issues. The stylomastoid foramen is important for diagnosing facial nerve problems. Plicae semilunares, found in the knee, help us understand knee mechanics.
Doctors and surgeons need to know a lot about these parts. Knowing how they work helps treat conditions like Bell’s palsy and plica syndrome. This knowledge is vital for good care.
Studying these parts shows how complex and fascinating our bodies are. More research will help us understand their roles in health and disease. This will lead to better care for patients.