The gastric cardia is a key part of our body. It links the esophagus to the stomach. This is important for our digestion.
At the bottom of the esophagus, the gastric cardia lets food move into the stomach. This is where digestion really starts.
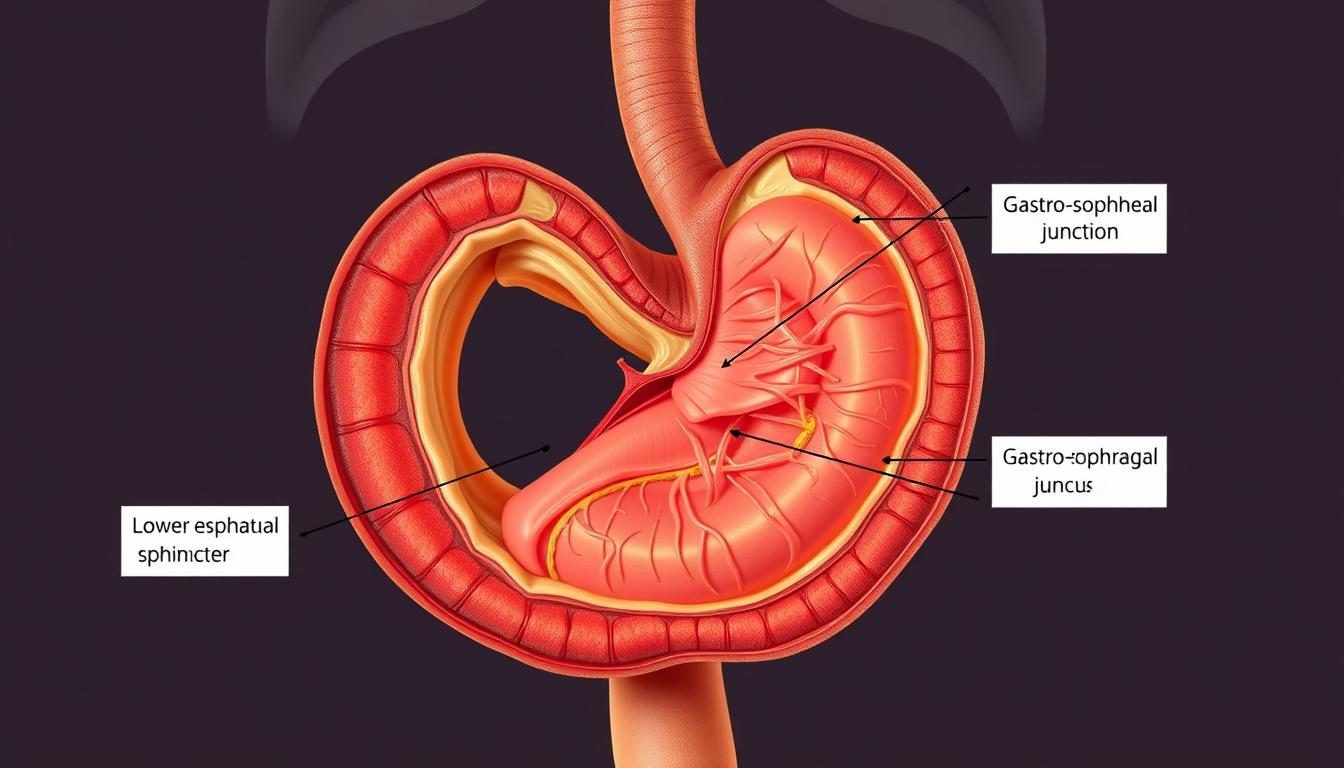
Knowing about the gastroesophageal junction and stomach anatomy helps us understand the gastric cardia. It’s a vital part that makes sure food moves right from the esophagus to the stomach.
Anatomical Structure of the Gastric Cardia
The gastric cardia is at the gastroesophageal junction. It’s a key area for digestion. It connects the esophagus to the stomach with unique features.
Location and Boundaries
The gastric cardia is where the esophagus meets the stomach. Its edges are not clear-cut. They mark where the esophageal and gastric mucosas meet.
Histological Composition
The gastric cardia’s makeup is important. It has epithelial layers that line it. These layers are essential for its role.
Epithelial Layers
The epithelial layer is mostly mucus-secreting cells. It shields the deeper tissues from stomach acid.
Glandular Components
The cardia has cardial glands. These glands are mainly mucous-secreting. They help build a protective mucous layer.
| Component | Description | Function |
|---|---|---|
| Epithelial Layer | Mucus-secreting cells | Protective barrier against gastric acid |
| Cardial Glands | Tubular glands with mucous-secreting cells | Contribute to mucous barrier |
Embryological Development of the Gastric Cardia
Understanding the embryological development of the gastric cardia gives us insights into its role. This area develops through a complex series of steps. These steps involve many cellular and molecular events working together.
Fetal Formation Stages
In fetal development, the gastric cardia starts from the foregut. This stage is when endodermal cells turn into the stomach and esophagus lining. The fetal formation stages are key in setting the boundary between the esophagus and stomach.
Developmental Milestones
Important developmental milestones include the growth of the gastric cardia’s muscular layer. Also, the development of its nerve connections is vital. These steps are essential for the gastric cardia to work right, like stopping stomach acid from going up.
The gastric cardia keeps growing and changing until birth. Big changes happen in the weeks before a baby is born.
Physiological Functions of the Gastric Cardia
The gastric cardia is a key part of the stomach. It has many important jobs. It helps keep the digestive system working right.
Secretory Activities
The gastric cardia makes mucus. This mucus shields the stomach from acid. It stops damage and keeps inflammation away.
Barrier Function
The gastric cardia protects the esophagus and stomach. It does this in several ways.
Protection Against Reflux
It stops stomach acid from going back up into the esophagus. This helps avoid problems like esophagitis.
Mucosal Defense Mechanisms
The gastric cardia also keeps the stomach lining safe. It makes mucus and bicarbonate. These help neutralize acid and keep the lining strong.
In short, the gastric cardia does a lot. It makes mucus and acts as a barrier. This protects against acid and keeps the stomach lining safe.
Gastroesophageal Junction Regulation
The cardioesophageal sphincter acts like a door to the stomach. It controls when food can enter the stomach. This area has many mechanisms to work well together.
Pressure Dynamics
Pressure at the gastroesophageal junction is key to its function. The lower esophageal sphincter (LES) keeps a high pressure. This stops stomach acid from coming back up.
This pressure changes based on:
- Muscle tone
- Neural inputs
- Hormonal signals
Sphincter Mechanisms
The sphincter mechanisms are vital for the gastroesophageal junction. The LES relaxes to let food in and tightens to keep acid out. This balance is important for:
- Food to pass into the stomach
- Preventing stomach acid from coming back up
- Keeping the esophagus healthy
In summary, the gastroesophageal junction’s regulation is a balance of pressure and sphincter actions. It ensures food moves into the stomach right and keeps acid out.
Neurological Control of the Gastric Cardia
The nervous system plays a key role in how the gastric cardia works. It’s all about balance. This balance is what keeps the cardia from letting stomach acid back up, while also letting food down.
Vagal Innervation
The vagus nerve is a big player in controlling the gastric cardia. It sends signals to the cardia, affecting how it works. Vagal stimulation can change the tone of the lower esophageal sphincter, which impacts reflux.
Enteric Nervous System Influence
The enteric nervous system (ENS) also has a big impact on the gastric cardia. It can work on its own to some extent. Local reflexes in the ENS can adjust the cardia’s function based on what’s inside, showing its ability to adapt.
Local Reflexes
Local reflexes in the gastric cardia are key for quick responses to changes. These reflexes can change the cardia’s tone and secretions. For example, food can trigger reflexes that help it move into the stomach.
Hormonal Regulation of Cardia Function
Gastric cardia function is controlled by many hormonal signals. These hormones are key for the cardia to work right. They help with both its secretions and its protective barrier.
Gastrin Effects
Gastrin is a hormone that impacts the gastric cardia. It makes the stomach produce more acid and helps the stomach lining grow. Gastrin receptors in the cardia show its role in controlling its function.
Other Regulatory Peptides
Other peptides also play big roles in the gastric cardia. Somatostatin and ghrelin are two examples. They have different effects on the cardia.
Somatostatin
Somatostatin slows down stomach acid release. It also helps control other hormone releases. Its presence in the cardia suggests it helps manage its function.
Ghrelin
Ghrelin is known for controlling hunger. It also affects how the stomach moves and its barrier function. This hormone is important for the cardia’s health.
| Hormone | Effect on Gastric Cardia |
|---|---|
| Gastrin | Stimulates gastric acid secretion |
| Somatostatin | Inhibits gastric secretion |
| Ghrelin | Influences gastric motility and barrier function |
The balance of these hormones is vital for the gastric cardia’s normal function. Knowing their roles helps us understand cardia disorders better.
Mucosal Protective Mechanisms
The mucosa of the gastric cardia has developed strong defense strategies. It is located at the junction of the esophagus and stomach. This area is exposed to acidic gastric contents, making it vulnerable to injury.
Mucus Production is key to protecting the mucosa. The gastric cardia’s mucosa creates a thick mucus layer. This layer acts as a barrier against acid and irritants. The mucus is rich in glycoproteins, which enhance its protective qualities.
Mucus Production
Mucus production is a continuous process. The mucus layer is constantly being secreted and shed. This turnover is vital for the mucosal barrier’s integrity. Disruptions, like Helicobacter pylori infection or NSAID use, can harm the mucosa.
Bicarbonate Secretion
The gastric cardia’s mucosa also secretes bicarbonate. This helps neutralize gastric acid. Bicarbonate secretion is a critical mechanism against acid-induced injury. Together, mucus and bicarbonate create a protective barrier. This barrier keeps the mucosal surface near-neutral pH, despite the stomach’s acidic environment.
Epithelial Regeneration
Epithelial regeneration is essential for mucosal protection. The epithelial cells of the gastric cardia regenerate quickly. This regenerative ability is vital for maintaining mucosal integrity and preventing complications like ulcers or strictures.
In summary, the gastric cardia’s mucosal protection involves mucus production, bicarbonate secretion, and epithelial regeneration. Understanding these mechanisms is key to grasping gastric cardia disorders. It also helps in developing effective treatments.
Vascular Supply and Microcirculation
The blood flow to the gastric cardia is key to its health. It helps the cardia work right, like stopping stomach acid from going up. This is important for keeping the stomach and esophagus healthy.
Arterial Network
The blood to the gastric cardia comes from the gastric arteries. These arteries make a network that brings oxygen to the cardia. The left gastric artery and right gastric artery are the main blood sources.
Venous Drainage
The blood from the gastric cardia goes to the gastric veins. These veins then flow into the portal vein. This system is vital for removing old blood from the cardia.
Lymphatic System
The lymphatic system of the gastric cardia helps fight off infections. Lymph from the cardia goes to the gastric lymph nodes and then to the celiac lymph nodes. This is important for the immune system to watch over the area.
Role in Digestion and Absorption
The gastric cardia is key in the early stages of digestion. It’s where food first meets the digestive system. This kickstarts the process that continues in the stomach and beyond.
The cardia region starts food processing early on. It’s vital for the body to absorb nutrients well later on.
Initial Food Processing
At the gastric cardia, food mixes with saliva and other oral secretions. This starts breaking down carbs. Even though the cardia doesn’t make digestive enzymes, it helps food move into the stomach. There, stomach juices break down the food further.
Contribution to Gastric Emptying
The gastric cardia also controls how fast food moves into the stomach. This affects gastric emptying. The speed at which food leaves the stomach impacts digestion and nutrient absorption.
| Function | Description | Impact on Digestion |
|---|---|---|
| Initial Food Processing | Mixing food with saliva and oral secretions | Prepares food for further digestion |
| Gastric Emptying | Regulating food flow into the stomach | Influences digestion and absorption rates |
In conclusion, the gastric cardia is vital for digestion’s early stages. It plays a big role in the digestive process, including gastric emptying and nutrient absorption.
Pathophysiology of Gastric Cardia Disorders
Gastric cardia disorders come from complex interactions. These include inflammation and changes that can lead to cancer. If not treated quickly, these issues can cause serious health problems.
Inflammatory Conditions
Helicobacter pylori infection is a big cause of inflammation in the gastric cardia. It can cause long-term inflammation and raise the risk of cancer. Other factors like gastroesophageal reflux disease (GERD) and what we eat also play a role.
“Chronic inflammation in the gastric cardia region can lead to mucosal damage and increase the risk of neoplastic transformations.”
Neoplastic Transformations
Changes in the gastric cardia can lead to adenocarcinoma, a serious cancer. This cancer is hard to treat. It develops due to genetics, environment, and long-term inflammation.
Adenocarcinoma Development
Adenocarcinoma in the gastric cardia means abnormal growth of glandular cells. This usually starts with long-term inflammation and changes in cell type.
Risk Factors
Many things can increase the risk of adenocarcinoma in the gastric cardia. These include chronic H. pylori infection, being overweight, and certain diets. Eating too much salt and not enough fruits and veggies are bad.
| Risk Factor | Description | Relative Risk |
|---|---|---|
| H. pylori infection | Chronic infection leading to inflammation | High |
| Obesity | Increased pressure on the gastric cardia | Moderate |
| Dietary factors | High salt, low fruit and vegetable intake | Moderate |
Gastroesophageal Reflux Disease and the Cardia
It’s important to know how the gastric cardia and gastroesophageal reflux disease (GERD) are connected. GERD happens when the sphincter at the top of the stomach relaxes too much. This lets stomach acid flow back up into the esophagus.
Pathophysiological Mechanisms
The way GERD works involves many parts. These include the gastric cardia, the lower esophageal sphincter (LES), and the lining of the esophagus. The main causes are:
- Transient LES relaxations
- LES hypotension
- Anatomical disruption of the gastroesophageal junction
Structural Alterations
Changes in the area where the stomach meets the esophagus can lead to GERD. These changes are:
- Hiatus hernia
- Shortening of the LES
- Alterations in the gastric cardia mucosa
Clinical Manifestations
GERD shows up in different ways. These include:
- Heartburn
- Regurgitation
- Dysphagia
- Chest pain
To manage GERD well, we need to understand these symptoms and why they happen.
Barrett’s Esophagus and Cardia Involvement
Barrett’s esophagus is a condition that can lead to esophageal cancer. It happens when the lining of the esophagus changes due to acid reflux. This change can spread to the stomach’s upper part, known as the cardia.
Metaplastic Changes
Changes in Barrett’s esophagus are a big worry because they can turn into cancer. The lining of the esophagus changes to a type that’s not normal. This is often because of long-term acid reflux.
- Incomplete Metaplasia: This type has goblet cells, showing a higher risk of turning into cancer.
- Complete Metaplasia: This type doesn’t have as many goblet cells and is less risky.
Dysplastic Progression
The progression of Barrett’s esophagus involves changes in genes and cells. It starts with non-dysplastic changes and can move to low-grade and then high-grade dysplasia. Each step increases the risk of cancer.
- Low-grade dysplasia: Shows a mild abnormality in cells.
- High-grade dysplasia: Shows a more serious abnormality, close to becoming cancer.
Surveillance Strategies
Keeping an eye on patients with Barrett’s esophagus is key. Regular check-ups with endoscopy and biopsies help catch problems early.
Surveillance Guidelines suggest:
- Endoscopy with biopsies for those without dysplasia.
- More frequent checks for those with dysplasia, based on its grade.
- Treatment for high-grade dysplasia or early cancer.
Understanding the changes and using the right check-ups can help doctors better care for patients with Barrett’s esophagus.
Helicobacter Pylori Infection at the Cardia
The gastric cardia is a key area where Helicobacter pylori infection can cause big problems. This bacterium leads to inflammation and raises the risk of stomach cancer.
Colonization Patterns
H. pylori can colonize the cardia in different ways, affecting how severe the infection is. Research shows that how dense H. pylori is in the area relates to the inflammation and damage to the mucosa.
Inflammatory Response
The presence of H. pylori at the gastric cardia starts an inflammatory response. This can lead to chronic gastritis and even more serious issues. The inflammation is marked by neutrophils and lymphocytes moving into the mucosa.
Long-term Consequences
The long-term effects of H. pylori infection at the cardia are serious, including a higher risk of gastric cancer. It’s important to understand how H. pylori colonizes and triggers inflammation to manage and prevent these outcomes.
| Condition | H. pylori Prevalence | Inflammatory Response |
|---|---|---|
| Gastritis | High | Severe |
| Gastric Cancer | High | Chronic |
| Normal Mucosa | Low | Minimal |
Diagnostic Approaches for Cardia Assessment
Checking the gastric cardia needs a mix of endoscopy, histopathology, and functional tests.
Endoscopic Evaluation
Endoscopy is key for seeing the gastric cardia. It lets doctors look at the mucosa and find any issues. High-definition endoscopy spots small changes, and narrow-band imaging shows blood vessels and odd mucosa.
Histopathological Analysis
Looking at biopsy samples from endoscopy is vital. It finds inflammation, dysplasia, and cancer in the gastric cardia.
Functional Testing
Functional tests show how the gastric cardia works. They include:
- pH monitoring to see acid levels
- Manometry to check muscle movement and sphincter strength
pH Monitoring
pH monitoring checks acid levels in the esophagus and gastric cardia. It spots GERD and checks if treatments work.
Manometry
Manometry looks at the esophagus and sphincter pressure. It tells us about the gastric cardia’s function.
| Diagnostic Approach | Description | Clinical Utility |
|---|---|---|
| Endoscopic Evaluation | Direct visualization of the gastric cardia | Detection of mucosal abnormalities and lesions |
| Histopathological Analysis | Examination of biopsy specimens | Diagnosis of inflammatory, dysplastic, and neoplastic conditions |
| pH Monitoring | Quantification of acid exposure | Diagnosis of GERD and assessment of acid-suppressive therapy |
| Manometry | Measurement of esophageal and LES pressure | Evaluation of motility and sphincter function |
Therapeutic Management of Cardia Disorders
Managing gastric cardia disorders requires a mix of treatments. It’s important to understand the disorder and what the patient needs.
Pharmacological Interventions
Medicines are key in treating cardia disorders. Proton pump inhibitors (PPIs) help by reducing stomach acid. This relieves symptoms of GERD.
“PPIs have changed how we treat GERD,” says a top gastroenterologist. “They effectively lower acid levels.” Other drugs, like histamine-2 (H2) blockers and antacids, also help manage symptoms.
Endoscopic Treatment Options
Endoscopic treatments are less invasive for cardia disorders. Radiofrequency ablation and endoscopic mucosal resection treat conditions like Barrett’s esophagus.
A study in a top medical journal shows endoscopic treatments improve Barrett’s esophagus outcomes.
Surgical Approaches
Surgery is sometimes needed for cardia disorders. Fundoplication strengthens the lower esophageal sphincter to treat GERD. For severe obesity or other issues, gastric bypass surgery might be considered.
A recent clinical guideline stresses the need for a team approach. Combining medicines, endoscopy, and surgery helps tailor treatments to each patient.
Emerging Research in Gastric Cardia Physiology
New studies are changing how we see the gastric cardia’s part in our gut’s health. Thanks to new research tools and methods, scientists can now study this area more closely.
Molecular Insights
At the molecular level, research is uncovering the complex ways the gastric cardia works. Scientists have found certain genes and proteins that are key to its function. For example, specific mucins and tight junction proteins help keep the barrier strong.
Novel Biomarkers
New biomarkers are helping doctors diagnose and track gastric cardia problems. Researchers are looking at cytokines and inflammatory mediators to see if they can predict disease and how well treatments will work.
Therapeutic Targets
Research is also finding new targets for treating gastric cardia diseases. By learning about the molecular pathways involved, scientists can create better, more focused treatments.
The future of gastric cardia research looks bright. With new tools and methods, we can expect big leaps forward in understanding and treating related disorders.
Conclusion
The gastric cardia is key to keeping the digestive system working right. Its structure, how it develops, and its functions are all linked to good digestion. This is important for our health.
When the gastric cardia doesn’t work right, it can cause problems like acid reflux and Barrett’s esophagus. Knowing how it works helps doctors find and treat these issues.
New research has given us a better understanding of the gastric cardia. It has found new ways to look at its functions and found markers for health issues. This is good news for finding new treatments.
In short, the gastric cardia is very important for our digestion. Problems with it can lead to serious health issues. More research will help doctors find better ways to diagnose and treat these problems, making patients’ lives better.