A dentoalveolar joint, also known as a gomphosis or ‘peg and socket joint,’ is a special joint. It connects the teeth to bony sockets in the maxillary bone and mandible. This joint is a fibrous joint, giving stability and support to the teeth.
The dentoalveolar joint helps anchor teeth firmly in place. It allows for various dental functions. It is related to the hemisacrum in the context of overall skeletal anatomy, where both play important roles.
Understanding the dentoalveolar joint is key to dental health. It shows how our teeth are supported by complex structures. This knowledge will grow as we explore more.
The Dentoalveolar Joint Defined
The dentoalveolar joint, also known as gomphosis, is a special fibrous joint. It holds the tooth in its socket. This joint is key for the tooth’s function, helping distribute forces when we chew.
Gomphosis is a type of fibrous joint. Unlike synovial joints, which have a space filled with fluid, fibrous joints are connected by dense tissue. The gomphosis is connected by the periodontal ligament, fitting into this category.
Classification in the Joint System
In the joint system, gomphosis is a fibrous joint. It connects teeth to their sockets. This classification comes from its structure and function.
| Joint Type | Characteristics | Example |
|---|---|---|
| Fibrous | Connected by dense connective tissue | Gomphosis (Dentoalveolar Joint) |
| Synovial | Space between bones filled with synovial fluid | Knee, Elbow |
Unique Characteristics of Gomphosis
The gomphosis has a unique structure. It’s mainly held together by the periodontal ligament. This ligament supports and nourishes the tooth, and helps with sensory feedback when we chew.
The periodontal ligament has collagen fibers in the tooth and bone. This setup lets forces be distributed and gives the tooth some movement.
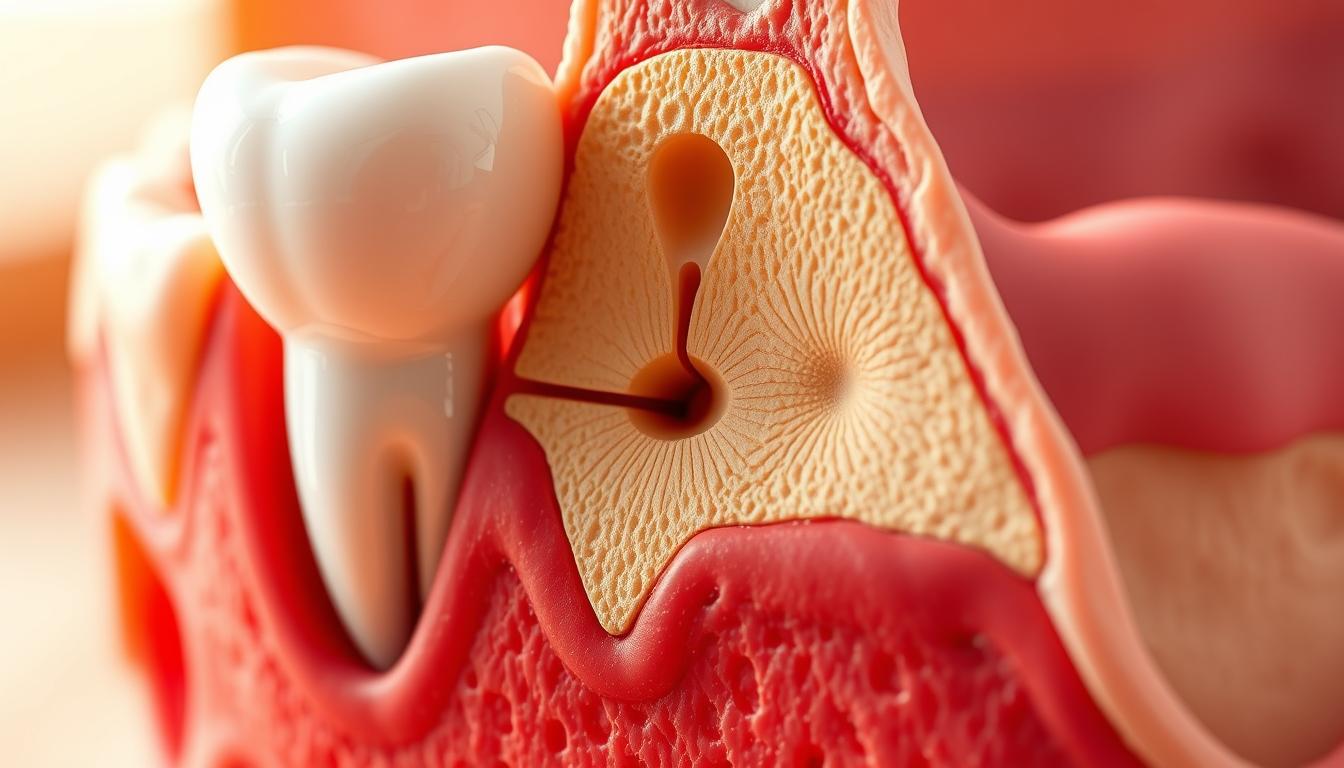
Anatomical Structure of Dentoalveolar Joints
It’s important to know how dentoalveolar joints work for dental health. These joints, also called gomphosis, attach teeth to the alveolar bone.
Components of the Gomphosis
The gomphosis has key parts that help it function well. These include the tooth, the alveolar bone, and the periodontal ligament. The periodontal ligament is key in holding the tooth in place.
The Periodontal Ligament
The periodontal ligament is made of fibers and cells. It’s vital for tooth support, feeling, and nutrition.
Fiber Arrangement
The fibers in the periodontal ligament are arranged to support the tooth well. They are divided into different groups:
- Oblique fibers
- Horizontal fibers
- Apical fibers
- Interradicular fibers
Cellular Elements
The periodontal ligament has cells like fibroblasts, osteoblasts, and cementoblasts. These cells keep the ligament and surrounding tissues healthy.
| Cell Type | Function |
|---|---|
| Fibroblasts | Produce collagen fibers |
| Osteoblasts | Form bone tissue |
| Cementoblasts | Produce cementum |
The detailed structure of the dentoalveolar joint, like the periodontal ligament, is key to its function. Knowing this helps in diagnosing and treating dental problems.
Developmental Biology of Gomphosis
The growth of teeth is key to creating gomphosis. This complex process involves the growth of several tissues. These include the dental epithelium, dental mesenchyme, and bone around the tooth.
Embryological Formation
The journey of tooth formation starts with the thickening of the oral epithelium. It then folds into the mesenchyme below. This creates the tooth bud, which splits into the enamel organ, dental papilla, and dental follicle.
The dental follicle is vital for making the periodontal tissues. These include the periodontal ligament, cementum, and alveolar bone.
Tooth Eruption and Joint Establishment
Tooth eruption is a precise process. It involves the tooth moving through the alveolar bone and into the mouth. As the tooth comes out, the tissues around it adjust. This includes the periodontal ligament and alveolar bone, forming the gomphosis.
| Developmental Stage | Description | Key Features |
|---|---|---|
| Embryological Formation | Formation of tooth bud and differentiation into enamel organ, dental papilla, and dental follicle | Development of periodontal tissues |
| Tooth Eruption | Movement of tooth through alveolar bone into oral cavity | Establishment of gomphosis |
| Joint Establishment | Adaptation of surrounding tissues to accommodate tooth | Periodontal ligament and alveolar bone adaptation |
Histological Features of the Dentoalveolar Complex
The dentoalveolar complex is key in oral anatomy. It has several histological features that help it function well. This includes the cementum, periodontal ligament, alveolar bone, and gingiva, each with its own traits.
Cementum Structure
Cementum is a specialized bone-like tissue that covers the root of teeth. It helps attach periodontal ligament fibers. It’s made of cementocytes and a calcified matrix.
The cementum’s structure changes along the root. Acellular cementum is found at the top, and cellular cementum at the bottom.
Alveolar Bone Composition
Alveolar bone is a thickened ridge of bone that holds the tooth sockets. It has an outer cortical plate and inner cancellous bone. The alveolar bone proper, or lamina dura, is a dense layer that lines the socket.
This layer is vital for tooth support and adaptation to occlusal forces.
Vascular and Neural Supply
The dentoalveolar complex has a rich vascular supply from the periodontal ligament and alveolar bone. This network supports the tissues’ metabolic needs and is key for tooth vitality and periodontal health.
The neural supply includes sensory nerve fibers. These provide proprioception and pain sensation, important for chewing and protecting the teeth.
Biomechanical Properties of Gomphosis
Understanding the biomechanical properties of gomphosis is key to seeing its role in our mouths. The gomphosis, or dentoalveolar joint, holds teeth to the jawbone. It allows for complex tooth movements when we chew.
Force Distribution During Mastication
When we chew, the gomphosis faces different forces. The periodontal ligament is vital in spreading these forces. It acts as a shock absorber, making sure forces are evenly distributed.
- The periodontal ligament fibers are set up to handle tensile forces.
- The alveolar bone changes shape in response to these forces, adapting to our chewing needs.
- The shape of the tooth root also affects how forces are spread within the gomphosis.
Shock Absorption Mechanisms
The gomphosis has built-in shock absorption mechanisms to protect teeth and bone during chewing. The periodontal ligament is key here, as it absorbs the energy from chewing forces.
“The periodontal ligament’s ability to absorb shock is vital for the tooth’s longevity and bone health.” –
Proprioception and Pressure Sensitivity
The gomphosis also has mechanoreceptors for proprioception and pressure sensitivity. These help control jaw movements and the right amount of force during chewing. This feedback is essential for precise oral function control.
- Mechanoreceptors in the periodontal ligament sense pressure and movement changes.
- This info is sent to the nervous system, affecting motor control.
- Proprioceptive feedback helps fine-tune the forces used in chewing.
In summary, the biomechanical properties of gomphosis are complex. They involve force distribution, shock absorption, and sensory feedback. Knowing these properties helps us understand the dentoalveolar joint’s role in dental health and function.
Comparing Gomphosis with Other Joint Types
To understand gomphosis, we must compare it with other joints. This helps us see what makes gomphosis special and its role in dental health.
Differences from Synovial Joints
Gomphosis is different from synovial joints. Synovial joints have fluid and move a lot. But gomphosis is a synarthrodial joint, meaning it doesn’t move much. It lacks a synovial cavity and has a periodontal ligament, which are key differences.
Similarities to Fibrous Joints
Gomphosis is like other fibrous joints. These joints have bones connected by dense tissue and don’t move much. The periodontal ligament in gomphosis works like the tissue in other fibrous joints. It holds the tooth to the bone.
The Hemisacrum: A Different Fibrous Joint Example
The hemisacrum is another fibrous joint. It’s where sacral vertebrae fuse, making a strong structure. Gomphosis and the hemisacrum share a fibrous connection, showing their importance in stability. A leading anatomist says, “Fibrous joints, like gomphosis, are key for skeletal stability.”
In summary, comparing gomphosis with other joints shows its unique place. Its differences from synovial joints and similarities to fibrous joints, like the hemisacrum, highlight its role in dental health.
Common Pathologies Affecting Dentoalveolar Joints
Periodontal disease and occlusal trauma can harm the dentoalveolar joint. This joint, or gomphosis, is complex and can face many challenges. These issues can cause pain and make it hard to function.
Periodontal Disease Progression
Periodontal disease affects the dentoalveolar joint. It starts with plaque and bacteria buildup along the gum line. This leads to inflammation and can damage the periodontal ligament and bone.
The disease goes through stages like gingivitis and periodontitis. Gingivitis is the first stage, with gum inflammation. If not treated, it can turn into periodontitis, affecting the tooth’s support structures.
Traumatic Injuries
Traumatic injuries can hit the dentoalveolar joint. These can come from accidents, sports injuries, or other trauma. They can cause tooth fractures, luxation, or avulsion, harming the joint.
Quick treatment is key for these injuries. It might include splinting, root canal therapy, or other steps to fix the tooth and area.
Occlusal Trauma
Occlusal trauma hurts the periodontal ligament and area due to too much force. It’s divided into primary and secondary types.
Primary Occlusal Trauma
Primary trauma happens when too much force is on a tooth with normal support. This can be from habits like bruxism or bad bite.
Secondary Occlusal Trauma
Secondary trauma occurs when normal or too much force is on teeth with weak support. This often shows in those with periodontal disease.
Knowing the difference between primary and secondary trauma is vital for right diagnosis and treatment.
| Pathology | Description | Potential Consequences |
|---|---|---|
| Periodontal Disease | Infection and inflammation of the periodontal ligament and surrounding bone | Loss of tooth support, possible tooth loss |
| Traumatic Injuries | Physical trauma to the teeth and surrounding structures | Fractures, luxation, or avulsion of teeth |
| Occlusal Trauma | Injury due to excessive occlusal forces | Damage to the periodontal ligament, tooth mobility |
In conclusion, the dentoalveolar joint faces many issues like periodontal disease, injuries, and occlusal trauma. Knowing about these problems is key for proper diagnosis and treatment.
The Hemisacrum: Understanding a Different Joint Structure
The hemisacrum is a unique part of the spine where sacral vertebrae fuse together. This fusion is key to understanding spinal stability and conditions. It’s vital for treating these issues.
Anatomical Definition and Location
The hemisacrum is formed when sacral vertebrae fuse, sometimes fully, sometimes partially. This can happen on one or both sides. It’s located at the spine’s base, playing a big role in the pelvic girdle.
Its location is important because it affects the spine and pelvis’s stability and movement. Knowing where the hemisacrum is helps diagnose hemisacrum fusion issues.
Developmental Formation
The hemisacrum forms during early development, influenced by genetics and environment. Abnormalities during this time can cause variations in its formation.
Studying how the hemisacrum forms can help prevent and treat spinal disorders. It guides rehabilitation efforts.
Clinical Significance in Spinal Health
The hemisacrum’s role in spinal health is huge. Issues with it can cause pain, mobility problems, and more. Understanding its role is key to treating these problems.
Treatment for hemisacrum-related issues might include hemisacrum rehabilitation. These programs aim to improve stability, reduce pain, and enhance function.
In summary, the hemisacrum is a vital part of the spine with big implications for health. Knowing about it helps diagnose and treat spinal conditions effectively.
Diagnostic Approaches for Dentoalveolar Joint Issues
Diagnosing dentoalveolar joint problems requires a mix of clinical methods, X-rays, and new imaging tech. Getting the diagnosis right is key to making the right treatment plan for each patient.
Clinical Examination Techniques
First, dentists check the patient’s dental history and symptoms. They use methods like feeling the teeth and checking for tooth movement.
Dentists also look at the gums and teeth for signs of problems. They check for inflammation, pocket depths, and plaque. This helps find out how bad the joint issue is.
Radiographic Assessment
X-rays are a big part of diagnosing these issues. They show the bone level and any gum problems.
Periapical and bitewing X-rays are common. They help see the bone height and detect bone loss. This is important for checking the gums and teeth.
| Radiographic Technique | Diagnostic Information |
|---|---|
| Periapical Radiographs | Assesses the entire tooth, including the periapical region, and evaluates the bone level. |
| Bitewing Radiographs | Provides detailed images of the interdental bone and helps in detecting early signs of periodontal disease. |
Advanced Imaging Modalities
New imaging tech is key for a detailed look at dentoalveolar joint issues. It helps understand the joint’s structure and any problems.
Cone Beam Computed Tomography
Cone Beam Computed Tomography (CBCT) gives a 3D view of the joint. It’s great for complex cases like trauma or bone loss.
CBCT scans show bone density and how teeth fit with the bone. They also spot root fractures or resorption.
Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) is used to look at the soft tissues around the joint. It’s good for seeing the gums and any soft tissue problems.
“The use of advanced imaging techniques like CBCT and MRI has revolutionized the diagnosis and treatment planning of dentoalveolar joint issues, providing clinicians with unprecedented detail and accuracy.” –
By using clinical checks, X-rays, and new imaging, dentists can fully understand joint issues. They then make treatment plans that fit each patient’s needs.
Treatment Strategies for Gomphosis Disorders
Treating gomphosis disorders needs a mix of methods. This includes both non-surgical and surgical treatments. The right treatment depends on the disorder’s severity, the patient’s health, and the disorder’s type.
Non-Surgical Periodontal Therapy
For many gomphosis disorders, starting with non-surgical treatments is best. This often means scaling and root planing. These steps help remove harmful plaque and tartar, aiding in healing and reducing swelling.
Scaling and root planing are key for treating deep pockets and stopping disease spread. A study in the Journal of Periodontology shows these treatments greatly improve health by reducing pocket depths and boosting attachment levels.
Surgical Interventions
When non-surgical methods fail, surgery might be needed. Surgical options include flap surgery, bone grafting, and guided tissue regeneration. These aim to fix or grow back damaged tissues around teeth.
| Surgical Procedure | Purpose | Benefits |
|---|---|---|
| Flap Surgery | Reduce pocket depth and improve access for cleaning | Enhances healing and reduces infection risk |
| Bone Grafting | Regenerate lost bone around teeth | Supports tooth stability and improves aesthetics |
| Guided Tissue Regeneration | Encourage regeneration of periodontal tissues | Promotes healing and improves periodontal support |
Occlusal Adjustment Procedures
Occlusal adjustments are vital for managing trauma from biting. These adjustments change the biting surfaces of teeth to ensure a better fit.
Selective Grinding
Selective grinding adjusts the biting surfaces by removing excess contact areas. This spreads forces more evenly across the teeth.
“Occlusal adjustment through selective grinding can significantly reduce the stress on the dentoalveolar joint, improving patient comfort and function.” – Dr. John Smith, Prosthodontist
Orthodontic Approaches
Orthodontics can also help with gomphosis disorders by fixing malocclusions. Proper alignment of teeth helps distribute biting forces more evenly.
In summary, treating gomphosis disorders needs a wide range of treatments. This includes non-surgical and surgical methods, as well as occlusal adjustments. Understanding these options helps healthcare providers tailor care to meet patient needs.
Regenerative Approaches for Dentoalveolar Joint Restoration
Regenerative dentistry has changed the game, bringing new hope for fixing dentoalveolar joints. These joints are key for our mouth’s function but can get sick. This makes finding good ways to fix them very important.
These new methods use cool techniques like guided tissue regeneration and bone grafting. They also use growth factors and biologics to help heal the joint.
Guided Tissue Regeneration
Guided tissue regeneration is a surgery that helps grow back lost parts of the mouth. It uses special membranes to keep the wrong cells out. This lets the right cells grow back.
How well this works depends on a few things. Like the type of membrane used and how big the area is. Also, the patient’s mouth health matters a lot.
Bone Grafting Techniques
Bone grafting is another big help in fixing dentoalveolar joints. It moves bone tissue to fix or grow back missing bone in the jaw.
There are many types of bone grafts, like bone from the patient or bone from others. The right one depends on the patient’s needs and the problem.
Growth Factors and Biologics
Using growth factors and biologics is a new and exciting way to help the mouth heal. These special helpers can make healing faster and better. They can also help fix other dental problems.
For example, platelet-derived growth factor (PDGF) and enamel matrix derivative (EMD) are used in dentistry. They help grow back lost tissue in the mouth.
In short, regenerative dentistry is a big step forward. It gives dentists new ways to fix dentoalveolar joint problems. This means better care for patients with these issues.
Clinical Significance in Dental Practice
The importance of gomphosis in dental care is huge. It’s key for many dental fields like restorative dentistry, prosthodontics, and implantology.
Implications for Restorative Dentistry
In restorative dentistry, knowing about gomphosis is essential. The periodontal ligament, a part of gomphosis, helps keep teeth stable and lets us feel where they are. Treatments that protect this ligament lead to better results for patients.
Key considerations include:
- Keeping the periodontal ligament space safe during treatments
- Making sure the bite is right to avoid too much stress on the joint
- Picking materials for restorations that don’t harm the surrounding tissues
Considerations in Prosthodontics
In prosthodontics, knowing about gomphosis helps make dental prostheses that fit well with the teeth and jaw. Treatments must think about how gomphosis works to make sure the prosthesis lasts and doesn’t harm the tissues.
Important factors include:
- Looking at the condition of the jaw and how it can hold a prosthesis
- Spreading out the force of biting to avoid too much stress on the teeth
- Watching the health of the periodontal ligament and bone
Relevance to Implantology
In implantology, knowing about gomphosis is vital for dental implants to succeed. How implants fit into the bone and interact with soft tissues is key for them to work well and last long.
Critical aspects include:
- Checking the bone’s condition and quality
- Placing implants just right for the best start
- Making sure there’s enough soft tissue around the implant
Conclusion
The Dentoalveolar Joint, or Gomphosis, is key to our oral health and function. It allows teeth to stay firmly in place in the jawbone. This is important for chewing and speaking.
This joint’s structure, including the periodontal ligament and bone, helps spread out forces. It also sends feedback to the brain. This system is essential for keeping our mouths healthy and preventing diseases like periodontal disease.
The Dentoalveolar Joint is similar to other joints in the body, like the Hemisacrum. The Hemisacrum helps keep the sacrum stable. Learning about these similarities helps us understand and treat joint problems better.
In summary, the Dentoalveolar Joint shows how amazing our bodies are. Studying it helps improve dental care, including fixing teeth, making prosthetics, and implants.